
Top AI Platforms for Healthcare Data Integration
Compare 10+ AI platforms that solve healthcare's data fragmentation problem and save hours on manual integration work.

Written by
Adam Stewart
Key Points
- Focus on HL7 and FHIR support over flashy AI features for real integration
- Start with read-only AI automation before enabling EHR write-back
- Demand confidence scores and clinician override capabilities
- Test compatibility with your existing 90+ EHR systems first
Healthcare data is scattered across over 90 electronic health record (EHR) systems and various platforms, creating challenges for providers. This fragmentation leads to inefficiencies, redundant tests, and risks to patient safety. AI platforms are addressing these issues by automating data standardization and integration, ensuring compliance with regulations like FHIR-based APIs and USCDI standards. Here's what to look for and the top platforms available:
Key Takeaways:
- Interoperability: Ensure support for HL7, FHIR, and other standards for seamless data exchange.
- AI Features: Look for natural language processing (NLP), terminology mapping, and automation for data normalization.
- Security & Scalability: Platforms must comply with HIPAA, offer encryption, and handle high data volumes efficiently.
Top Platforms:
- Enterprise Interoperability Platforms (e.g., Redox, Particle Health, Health Gorilla): Focus on connecting EHR systems and diagnostic data.
- Clinical Data Normalization Tools (e.g., Mirth Connect, Talend): Transform unstructured data into standardized formats.
- Cloud-Based Platforms (e.g., AWS HealthLake, Google Cloud Healthcare API): Combine data storage, AI analytics, and compliance.
Quick Comparison:
| Platform Type | Examples | Best Use Case |
|---|---|---|
| Enterprise Interoperability | Redox, Particle Health | Linking EHR systems, diagnostic networks |
| Clinical Data Normalization | Mirth Connect, Talend | Data standardization, terminology mapping |
| Cloud-Based Platforms | AWS HealthLake, Azure | Scalable AI-driven analytics and storage |
AI tools also streamline patient interaction data, converting calls and messages into actionable insights for better care coordination. Choosing the right platform ensures improved efficiency, compliance, and patient outcomes.
How to Evaluate AI Platforms for Healthcare Data Integration
When selecting an AI platform for healthcare data integration, it’s crucial to assess its technical capabilities, compliance measures, and overall fit for your organization. This involves leveraging reference customers, conducting proof-of-concepts, and analyzing capability matrices. By aligning these evaluation steps with the data challenges discussed earlier, you can ensure the chosen platform delivers both efficiency and compliance.
Interoperability Standards Support
One of the first things to verify is whether the platform supports key interoperability standards such as HL7 v2, HL7 v3, FHIR (R4 and emerging R5), C-CDA, DICOM, X12 (claims and eligibility), as well as U.S.-specific standards like USCDI and state immunization registry formats. These standards are essential for seamless integration with major systems like Epic, Cerner, and Athenahealth, as well as imaging systems, laboratories, and payers. Proper support minimizes the need for custom interfaces, enabling faster onboarding - like connecting a new lab in weeks instead of months - and reducing translation errors.
Ask vendors for a detailed matrix of supported standards and examples of real-world interfaces they’ve implemented. Pay close attention to the number of live healthcare connections they maintain and whether the platform can normalize data across HL7, FHIR, and C-CDA instead of just passing messages through. It’s also worth checking if the platform includes pre-built connectors for major EHRs, labs, imaging centers, and clearinghouses, along with tools for mapping, routing, and monitoring integrations. Dashboards, alerting features, and message replay capabilities are also important for managing these integrations effectively.
AI Features for Data Normalization and Automation
Beyond interoperability, robust AI capabilities are critical for managing healthcare data efficiently. Essential AI features include clinical natural language processing (NLP) for converting unstructured data - like notes, referral letters, and call transcripts - into structured formats. Look for entity extraction capabilities that can identify key elements such as problems, medications, labs, procedures, dates, and providers, all mapped to standard terminologies. Additionally, the platform should support terminology mapping for coding systems like SNOMED CT, LOINC, RxNorm, and ICD-10-CM, and ensure these mappings are maintained over time. Deduplication and record linkage tools are also crucial for merging duplicate records across various sources.
Optional but valuable features include anomaly detection and AI-driven data quality scoring, which can further enhance analytics and decision-making.
Transparency and safety controls are equally important. Does the platform provide explanations or confidence scores for matches, mappings, and flags, or does it function as a "black box"? Can clinicians or data stewards review and override automated decisions - like merges, mappings, or alerts - before they impact EHRs or patient care? Additionally, the platform should track AI model versions and allow rollbacks in case of incorrect mappings or merges. Many organizations start with AI automation in read-only or analytics pipelines, such as registries or quality reporting, before enabling write-back capabilities. Pilot programs can help monitor error rates and gather user feedback to refine these processes.
Security, Compliance, and Scalability
A reliable platform must adhere to HIPAA standards and be willing to sign a Business Associate Agreement (BAA). It should employ up-to-date encryption protocols like TLS 1.2+ and AES-256, while also supporting key management, OAuth 2.0/OpenID Connect, role-based access control (RBAC), and comprehensive audit trails. Additional network protections, such as private connectivity options, IP allowlists, and optional VPNs or private links, are also important. Request evidence of third-party assessments like SOC 2 Type II or HITRUST certifications and review how the platform handles PHI during development and model training.
Scalability is another critical factor. The platform should support high message throughput and manage large numbers of concurrent connections, which is essential for multi-hospital systems or national networks. It must handle real-time data streams like ADT feeds, lab results, imaging files, and claims without introducing latency that could disrupt clinical workflows. Look for elastic cloud scaling capabilities, published performance benchmarks, and references from organizations of similar size. Built-in mechanisms for queueing, retrying, and error handling are also essential to prevent data loss during traffic spikes or outages.
Top AI Platforms for Healthcare Data Integration
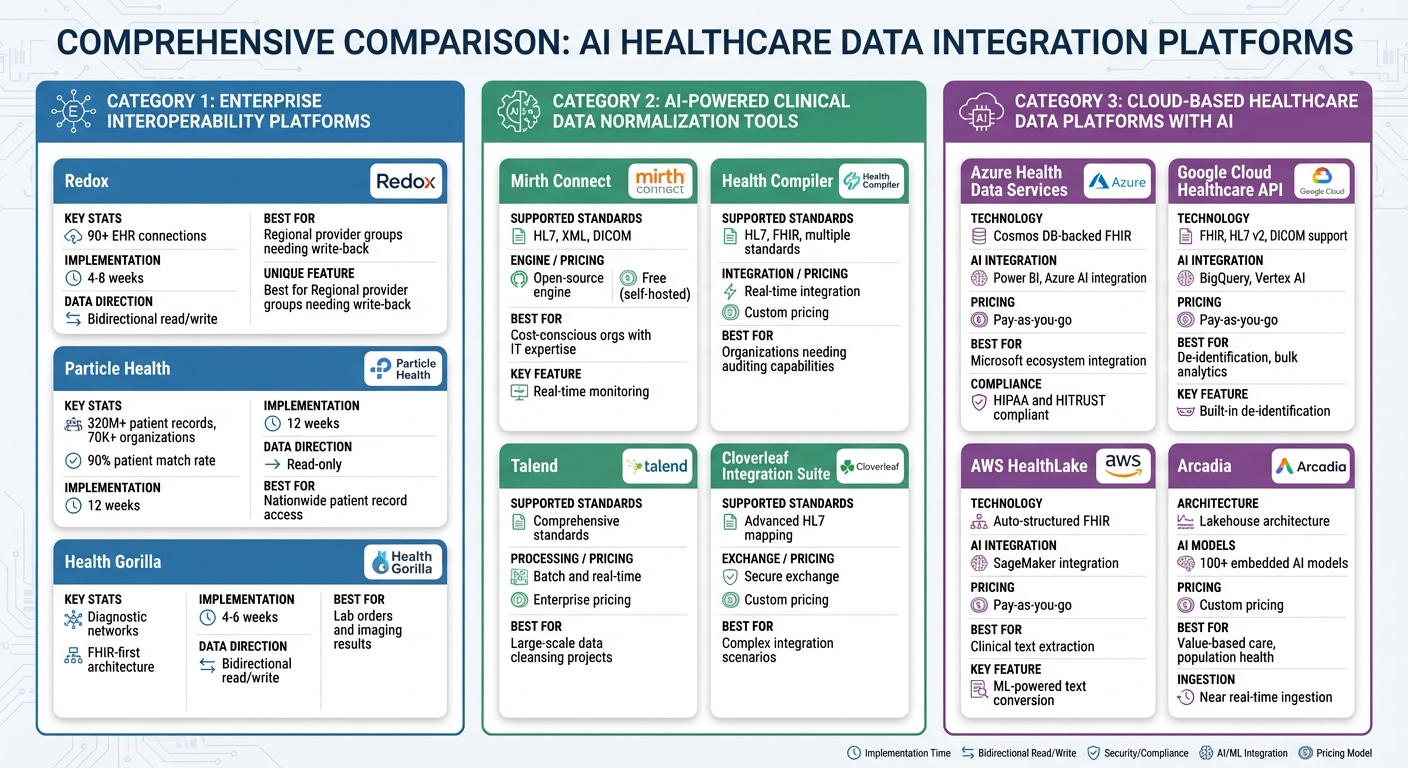
Comparison of Top AI Healthcare Data Integration Platforms by Type and Capabilities
In the U.S. healthcare market, there are several categories of AI-driven platforms designed to tackle specific data challenges. These include enterprise interoperability platforms for linking multiple EHR systems, clinical data normalization tools for cleaning and standardizing complex healthcare datasets, and cloud-based platforms that combine data storage with AI analytics. Choosing the right type of platform depends on your organization’s needs, as each addresses unique challenges while adhering to standards for interoperability, automation, and security.
Enterprise Interoperability Platforms
Enterprise interoperability platforms are built to efficiently connect various healthcare systems. For example:
- Redox provides connections to over 90 EHR systems, with the ability to normalize data formats like HL7, FHIR, and C-CDA. Implementation takes about 4-8 weeks [1].
- Particle Health aggregates more than 320 million patient records from 70,000+ organizations through HIE networks. It’s optimized for read-only data retrieval and offers a 90% patient match rate, with a 12-week implementation timeline [1].
- Health Gorilla focuses on diagnostic data exchange, using a FHIR-first architecture for lab orders and imaging results. Deployment typically takes 4-6 weeks [1].
| Platform | EHR Connections | Implementation Time | Best For | Read/Write |
|---|---|---|---|---|
| Redox | 90+ systems | 4-8 weeks | Regional provider groups needing write-back | Bidirectional |
| Particle Health | 320M+ records, 70K+ orgs | 12 weeks | Nationwide patient record access | Read-only |
| Health Gorilla | Diagnostic networks | 4-6 weeks | Lab orders and imaging results | Bidirectional |
For large health systems with nationwide reach and high diagnostic workloads, combining these platforms can offer a robust solution [1]. Each meets critical benchmarks for scalability and interoperability.
AI-Powered Clinical Data Normalization Tools
While enterprise platforms focus on system connectivity, clinical data normalization tools specialize in transforming raw, unstructured data into organized, usable formats. Some notable tools include:
- Mirth Connect: An open-source solution supporting HL7, XML, and DICOM. It offers message routing, data transformation, and real-time monitoring [2].
- Health Compiler: Provides real-time integration for standards like HL7 and FHIR, along with auditing capabilities and an intuitive interface [2].
- Talend: Focuses on data profiling and cleansing, supporting both batch and real-time integrations for large-scale projects [2].
- Cloverleaf Integration Suite: Features advanced HL7 mapping and routing, making it suitable for complex integration scenarios while ensuring secure data exchange [2].
| Platform | Terminology Support | Integration Methods | Cost Model | Best For |
|---|---|---|---|---|
| Mirth Connect | HL7, XML, DICOM | Open-source engine | Free (self-hosted) | Cost-conscious orgs with IT expertise |
| Health Compiler | HL7, FHIR, multiple standards | Real-time integration | Custom pricing | Organizations needing auditing capabilities |
| Talend | Comprehensive standards | Batch and real-time | Enterprise pricing | Large-scale data cleansing projects |
| Cloverleaf | Advanced HL7 mapping | Secure exchange | Custom pricing | Complex integration scenarios |
These tools are designed to meet the data normalization and terminology mapping needs outlined in industry evaluation standards.
Cloud-Based Healthcare Data Platforms with AI
For organizations looking for scalable, cloud-native solutions, these platforms integrate data storage, AI analytics, and compliance into a single offering:
- Microsoft Azure Health Data Services: Supports native FHIR with Cosmos DB for large-scale data storage, real-time analytics via Power BI, and compliance with HIPAA and HITRUST [4].
- Google Cloud Healthcare API: Offers support for FHIR, HL7 v2, and DICOM, with features like built-in de-identification and integration with BigQuery and Vertex AI for advanced analytics [4].
- AWS HealthLake: Leverages machine learning to convert clinical text into structured FHIR resources, creating searchable repositories for analytics and predictive modeling [5].
- Arcadia: A lakehouse-based platform that supports over 100 AI models, enabling near real-time ingestion and analysis of diverse data types at scale [5].
| Platform | FHIR Repository | AI/ML Integration | Pricing Model | U.S. Workflow Fit |
|---|---|---|---|---|
| Azure Health Data Services | Cosmos DB-backed | Power BI, Azure AI | Pay-as-you-go | Microsoft ecosystem integration |
| Google Cloud Healthcare API | Managed FHIR | BigQuery, Vertex AI | Pay-as-you-go | De-identification, bulk analytics |
| AWS HealthLake | Auto-structured FHIR | SageMaker integration | Pay-as-you-go | Clinical text extraction |
| Arcadia | Lakehouse architecture | 100+ embedded models | Custom pricing | Value-based care, population health |
Additionally, InterSystems Ensemble combines integration, data aggregation, and workflow automation in one platform, supporting standards like HL7, FHIR, X12, and DICOM [3]. For analytics, Innovaccer offers AI-driven population health insights with real-time data integration [6], while Arcadia Analytics specializes in value-based care and patient risk stratification [6]. These cloud platforms align with the security and AI automation requirements discussed earlier.
sbb-itb-ef0082b
AI Integration for Patient Interaction Data
AI is transforming how patient interaction data is handled, building on the foundation of system interoperability. While enterprise platforms excel at connecting systems, a large portion of healthcare data comes from patient phone calls, voicemails, and chat conversations - sources that are often unstructured and challenging to integrate. Today's AI platforms address this issue by converting these interactions into standardized formats that seamlessly integrate with EHRs, scheduling systems, and analytics tools, bridging a critical gap in healthcare data management.
Turning Patient Call Data into Usable Information
AI platforms excel at converting spoken interactions into structured, actionable data. Automatic Speech Recognition (ASR) transforms audio into text, using medical vocabularies to accurately capture clinical and insurance-specific terminology. Then, Natural Language Processing (NLP) steps in to identify key details - such as patient name, date of birth, reason for the call, preferred appointment time, insurance information, and symptom descriptions - and maps these to standardized fields aligned with HL7 and FHIR frameworks.
Here’s what gets extracted and organized: patient details (name, DOB, callback number), contact information (address, insurance details, preferred location), reasons for interaction (appointment requests, prescription refills, symptom reports), clinical context (symptom onset, severity, medications), and scheduling preferences (specific date/time windows in U.S. time zones, visit type). Once the data is validated using business rules to ensure completeness and proper formatting, it’s sent to EHRs and scheduling systems through APIs or FHIR resources like Patient, Appointment, and CommunicationRequest.
Take Dialzara, for example. This platform captures essential caller information and integrates it directly into healthcare workflows. Operating 24/7, it gathers caller identity and intent, organizes the information into discrete data elements, and integrates it with thousands of business applications. It also triages calls, separating urgent matters from routine inquiries, and generates call summaries that feed into clinical and operational workflows. This process creates consistent interaction records, enabling smoother scheduling and follow-ups.
Streamlining Workflows with AI Automation
Automating patient intake and scheduling with AI significantly improves efficiency. Primary care and urgent care clinics use AI agents to handle after-hours calls, summarizing symptoms and scheduling preferences into structured messages. These messages create draft appointments directly in scheduling systems, allowing staff to review and confirm instead of manually entering data. This reduces backlogs and missed calls. Specialty practices also benefit, as AI captures details like referring provider information, diagnoses, imaging history, and insurance data, which are then pushed into EHR referral modules, speeding up the process from referral to appointment.
AI eliminates common pain points like double entry, which reduces transcription errors (e.g., misspelled names or incorrect dates). Pre-validation ensures incomplete entries are flagged before they reach the EHR. Auto-routing assigns tasks to the correct work queues with full context, and standardized intake scripts guarantee that every caller is asked the same essential questions in the same order. One healthcare business using Dialzara reported an additional $16,000 in revenue within just a few months by capturing after-hours opportunities that would have otherwise been lost [7]. These platforms not only reduce administrative burdens and errors but also enhance data integration across communication channels and clinical systems.
Choosing the Right AI Platform for U.S. Healthcare Organizations
When it comes to integrating healthcare data, U.S. healthcare organizations need an AI platform that checks three crucial boxes: regulatory compliance, interoperability standards, and proven AI capabilities. Any platform must meet HIPAA security and privacy requirements, align with CMS quality and interoperability initiatives, and adhere to ONC information-blocking rules while supporting FHIR-based patient access APIs. Without these critical elements, organizations risk legal challenges, reimbursement penalties, and operational inefficiencies.
On the technical front, look for platforms that support key standards like HL7 v2, FHIR R4, C-CDA, X12, and DICOM. Advanced AI features are equally important - such as natural language processing (NLP) to extract structured data from clinical notes and calls, machine learning for patient matching and deduplication, and automated normalization to terminologies like SNOMED CT, LOINC, and RxNorm. These capabilities directly enhance data quality and streamline care coordination.
Scalability and robust security are non-negotiable. Cloud platforms with petabyte-scale processing, near real-time data ingestion, and secure multi-tenant architectures are essential to handle the increasing data loads from EHRs, wearable devices, telehealth platforms, and call centers - all without disrupting clinician workflows. Features like encryption, role-based access controls, audit trails, and Business Associate Agreements (BAAs) ensure compliance with HIPAA regulations.
Another often-overlooked layer is the patient interaction layer. A significant amount of healthcare data comes from phone calls, voicemails, and chat conversations - channels that traditional systems often fail to capture. AI tools like Dialzara address this gap by collecting patient intake details, appointment requests, and symptom descriptions around the clock. These tools transform voice interactions into structured, actionable data that seamlessly integrates with scheduling systems, CRMs, and EHR workflows, ensuring no critical information is missed.
A platform that combines these technical strengths with patient-focused capabilities lays the groundwork for better care coordination and financial outcomes. By aggregating clinical, claims, and social determinants data, such a platform supports value-based care programs. It enables risk stratification, identifies quality gaps, and benchmarks performance metrics tied to CMS contracts. Organizations that choose platforms meeting these criteria see tangible results: more complete patient records, fewer manual errors, and improved financial outcomes in value-based reimbursement models.
FAQs
What interoperability standards should I look for in an AI platform for healthcare data integration?
When selecting AI platforms for healthcare data integration, it's crucial to focus on interoperability standards that enable smooth data exchange and ensure systems work well together. Here are some of the key standards to keep in mind:
- HL7 FHIR (Fast Healthcare Interoperability Resources): A cutting-edge standard designed for the electronic exchange of healthcare information.
- HL7 v2 and CDA (Clinical Document Architecture): Commonly used standards for sharing clinical data and standardizing healthcare documents.
- DICOM: A must-have for handling and sharing medical imaging data efficiently.
- SNOMED CT: A clinical terminology system that ensures data is represented consistently and accurately.
By adhering to these standards, healthcare systems can enhance communication, maintain data accuracy, and achieve the level of interoperability needed to deliver better patient care.
How do AI tools like NLP and terminology mapping improve healthcare data integration?
AI tools such as natural language processing (NLP) and terminology mapping are transforming how healthcare systems manage complex medical language. These technologies simplify the interpretation and standardization of varied medical terminologies, making it easier for systems to communicate effectively and improving interoperability across platforms.
By breaking down barriers in medical jargon and aligning different data formats, these AI-powered solutions ensure healthcare providers have access to precise, consistent, and usable information. This not only streamlines workflows but also supports more informed decision-making, leading to improved patient care.
What key security and compliance features should an AI platform offer for safe healthcare data integration?
AI platforms working with healthcare data need to put security front and center. This means using tools like encryption - both while data is stored and during transmission - along with multi-factor authentication and strict access controls to shield sensitive patient information. Adhering to regulations like HIPAA is equally important to protect patient privacy, manage data securely, and maintain detailed audit trails.
Beyond these basics, platforms should also regularly assess their security systems, apply data anonymization methods, and rely on secure sharing protocols. These steps aren’t just about avoiding breaches - they’re about building trust and ensuring smooth, regulation-compliant data integration across the healthcare landscape.
Summarize with AI
Related Posts
HIPAA Compliance in AI Client Intake
Learn how AI client intake systems can maintain HIPAA compliance while enhancing data security and streamlining workflows.
HIPAA-Compliant AI Phone Agents for Healthcare
Explore how HIPAA-compliant AI phone agents enhance patient communication, ensuring security and efficiency in healthcare interactions.
5 AI Tools for HIPAA-Compliant Healthcare
Explore five AI tools designed for HIPAA-compliant healthcare, enhancing efficiency while safeguarding patient data.
How AI Improves Patient Data Analysis
AI is revolutionizing healthcare by enhancing patient data analysis for early disease detection, outcome prediction, and personalized treatment.
